The human foot has 26 bones, 33 joints, and more than 100 tendons, muscles, and ligaments. With such a complex structure, a lot can go wrong. While some foot problems are inherited, many occur because of years of wear and tear. Signs of foot trouble include pain, excessively dry skin, thickened or discolored nails, swelling, redness, and unusual sensations. “Consumers should know that these symptoms are not normal,” says Joshua Kaye, D.P.M, a podiatrist in Los Angeles. “Whatever the problem is, don’t bury it in your shoe and hope it will go away.”
Pain in the feet can trigger pain in the legs, hips, and back. Some foot problems can even signal a larger disease, which is why the American Podiatric Medical Association (APMA) suggests that people take their socks off when they go to their primary care physician for a regular checkup. In a recent APMA survey of more than 600 people, 73 percent said their feet were not routinely inspected at doctor visits.
Toenails that are rounded inward instead of outward could signal iron deficiency anemia. Kidney disease, heart disease, high blood pressure, and circulatory problems can cause the feet to swell. Tingling or numbness in the feet and slow healing wounds could be signs of diabetes or other serious diseases, according to the APMA. Chronic stiffness in the toes could be a sign of arthritis. “Changes in the structural appearance of the foot can also be signs of abnormalities such as tendon rupture, rheumatoid or osteoarthritis, or neuropathic disease,” says Barbara Buch, M.D.
- Avoid problems by wearing properly fitted shoes. If you feel discomfort or pain while wearing the shoes, it may be a sign to change shoes or consult a podiatrist.
- Shoes should fit comfortable the first time you try them on. You should not have to break them in.
- Early-stage conditions can often be successfully treated by switching to a better-fitting shoe that accommodates the problem.
- If the condition becomes chronic, surgery will often fix the condition.
For heel pain, orthotics in combination with exercise or physical therapy are successful in about 80 percent of cases. A recent innovation to treat heel pain is shockwave therapy, where the heel is bombarded with either high- or low-energy shockwaves to reduce the pain and inflammation.
Many people don’t consider sports-related foot discomfort serious in their early years. At issue with any discomfort for young athletes is the tendency to dismiss the pain as simply the price of activity or as a minor problem that will eventually pass. Sometimes the pain does goes away, although that doesn’t necessarily mean the same for the underlying condition. Sometimes the damage is accretive, meaning it builds up over time. Then, as we age, our feet become less flexible and recuperative, leading to the surfacing of conditions caused in earlier years.
Therefore, when it comes to sports at any age, its often better to have a podiatrist review the problem to determine its true severity.
Treatment of athlete’s foot includes topical anti-fungal medications and proper foot hygiene — drying between toes, proper use of medications and alertness to early warning signs. If untreated, the condition can also become a mixed bacterial/fungal infection that is much more difficult to treat. It can also lead to fungal nails, which are a thickening of the toenail and harder to treat a three-month regimen of Lamisil and additional months for the nails to regrow. Some doctors treat the condition with laser therapy, but its considered experimental and usually not covered by insurance.
A soft corn, which develops between toes, is quite prone to infection but easily treated with surgery. Because of the moisture between the toes, the corn is soft and absorbs the moisture and creates a foot odor, dermatitis and often a burning sensation.
Treatment of standard corns and calluses includes trimming them down to provide temporary relief and adjusting the shoes to relieve the pressure and irritation. The lesion should fade over time. But if the condition returns more frequently than every eight weeks or is particularly painful, surgery is recommended to ensure that the condition does not recur. Pain may be relieved by moleskin or padding. Corns and calluses should never be cut with an instrument by a non-physician, as this can lead to infections and other complications.
Treatment of ingrown nails starts with proper removal of the offending portion of nail. This is often all that is needed. In some cases, the condition returns. This can happen because the initial trimming is done at an angle to the root of the nail. If this procedure doesn’t cure the problem, the angle cut can increase the chance that the condition becomes more severe. The nail matrix (root) is not treated initially and is still as wide. So as the nail grows out, if the ingrown condition is due to ill-fitting shoes or another problem such as a fungal infection, then to fix the chronic problem, a simple surgery is needed to eliminate a part of the nail root to prevent problematic growth. The result is a slightly thinner nail, and the original problem will not reoccur.
Children are more susceptible than adults, in part because they more frequently walk barefoot on dirty surfaces. Sometimes the warts will disappear on their own over one to two months. If they don’t fade, however, treatments include surgically trimming the lesion or using various chemicals to induce the body to literally force the wart to fall off. In rare occasions, an untreated wart can proliferate into broader conditions of dozens or even hundreds of warts known as a mosaic, which is more difficult to treat.
A related condition is called porokeratosis, which Dr. Brady believes is a sweat gland on the bottom of the foot that becomes calloused. The condition goes further into the foot and often causes more discomfort than from a wart.
Diabetes causes hypersensitivity in some cases, but more often the patient loses sensation in the feet making them less responsive to a variety of conditions whose symptoms include pain such as hammertoe and bunions. If they aren’t seeing a podiatrist or other physician regularly, these conditions may become more serious before they are identified.
Diabetes is the leading cause of non-traumatic foot amputations each year. People with diabetes may experience neuropathy in the feet, a condition that affects the nerves and the ability to feel pain and heat or cold. “Someone without sensation in the feet can literally step on a nail and not know it,” says Amir Assili, D.P.M, a podiatrist in Gaithersburg, Md. Assili says a 28 year old man who came in complaining of a loss of sensation in both feet was diagnosed with diabetes soon after.
Another major foot problem linked to diabetes is poor blood circulation. High levels of blood sugar damage the blood vessels, making them less able to supply the skin and other parts of the body with blood. Poor circulation interferes with the ability to heal and raises the risk of infection. Minor cuts or even cracks from dry skin can turn into ulcers, small red sores that can become deep and infected. Foot amputations may be necessary when an infection reaches bone and spreads beyond a manageable extent.
Doctors normally treat diabetic foot ulcers by cleaning them and applying wound dressings, or with surgical debridement, which removes contaminated tissue from a wound to prevent infection. In severe cases, reconstructive procedures that reshape the foot may be needed to prevent undue pressure on the foot. During the past few years, the FDA has approved new products to treat chronic foot ulcers that are not responding to standard methods. Examples are Apligraf, made by Organogenesis Inc. of Canton, Mass., and Dermagraft, made by Smith and Nephew in La Jolla, Calif. “The optimal approach,” Assili says, “is to prevent ulcers from occurring through tight blood sugar control and regular visits to an endocrinologist.”
People with diabetes should also see a podiatric physician at least once a year and practice the basics of good foot care that apply to everyone: wearing comfortable socks and shoes and maintaining foot hygiene. Those who have been diagnosed with decreased circulation or neuropathy with loss of protective sensation should be seen by their podiatric physician more frequently. Feet should also be checked daily by the patient or family members for any cuts and sores. “Early detection is important because a problem can quickly turn serious,” Assili says. People with diabetes and other circulatory problems should never try to treat their own feet, because of the risk of infection.
Younger diabetics need to account for their increased risk of infection and of losing sensation in their feet. Many diabetics are eligible for an annual set of shoes fitted by a podiatrist and paid by the federal government, which has found that the shoes prevent serious and expensive conditions. Regular visits to a podiatrist, usually at least once a year, are an important element of caring for diabetes.
People also should purchase the right shoe for the sport. “Many injuries occur because someone is wearing a running shoe while playing basketball,” Losito says. Another common cause of athletic injuries is doing too much too soon. “Both overuse training habits and worn out shoes could result in stress fractures, heel pain or heel spur (plantar fasciitis) or shin splints,” he says. “It is important to start out slowly and increase distance, duration, and pace gradually. For runners, I recommend no more than a 10 percent increase per week.”
Walking or jumping on hard surfaces and failing to stretch and do warm ups may also cause shin splints, plantar fasciitis, and heel spurs. Losito says, “There is no solid evidence to confirm that stretching actually decreases the likelihood of injuries, but it makes sense to maintain flexibility through gentle stretching, especially following exercise.”
According to the American Academy of Podiatric Sports Medicine, the most common pain associated with jogging is runner’s knee, which can be caused by rolling in or down on the foot. With aerobics, rising on the toes can cause an inflamed Achilles tendon. Stress fractures can be caused by running and other repetitive strain. Sharp pain, bruising, or swelling after a foot injury warrant medical attention. Contrary to popular belief, it’s possible to walk, even if a foot bone is broken.
The two key components are stretching and support. You can augment support by either increasing control of the foot from below or reducing the load. If you are overweight a loss of as little as 5 pounds can give dramatic results. Foot supports or prescription orthotics control the foot from in the shoe. If you are in sever pain and this condition is interfering with your daily life see a Podiatrist immediately.
- Wear a good supportive shoe. This is a shoe with a rigid counter (The area of the shoe around the sides of the heel.) It should be difficult to press this area of the shoe in. Most New Balance® Sneakers are good examples of shoes with a rigid counter. I recommend all patients obtain tie shoes with a rigid counter in the correct width and length.
- Support the foot. First try OTCSpenco Arch Cushions® 3/4 length.
- Stretch the muscles and ligaments of the foot and lower leg at least twice daily.
- After using the above in combination for a week or two if you are still experiencing discomfort non-steroidal anti-inflammatory medications can be given.
- If there is less then a 50% improvement after month then it is time to see a doctor. Depending on the severity of the condition he may want X-rays or a Sonogram of the foot.
- A prescription custom orthotic may be necessary, and night splints prescribed to augment stretching.
50 % of patients are improved with stretching, the Spenco Arch Cushion combined with a rigid counter tie shoe in about 4 weeks.
Anti-inflammatory medication will hasten pain reduction. If after a month results are still not satisfactory a visit to a podiatrist is recommended. Prescription Orhtotics offer the best control of the foot. If pain persists, local steroid injections are often helpful. If you are overweight a serious attempt should have been made to reduce weight.
Surgical intervention should not be considered until the patient has failed at least 6 months of conservative therapy. Which includes an examination by a podiatrist; and use of prescription Orthotics (not over the counter shoe inserts) and stretching. I would also recommend ESWT treatment before surgery. If surgery is necessary it may include release of the plantar fascia, removal of the heel spur and or freeing up the nerve.
Basic Stretch for Achilles tendon and Plantar Fascia
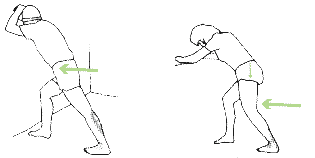 To stretch your calves stand a little away form a solid structure. Lean on your forearms, head resting on hands. Bend one leg and put that foot on the ground in front of you with the other leg straight behind you. Slowly move your hips forward keeping you lower back flat. Be sure to keep your back foot heel on the ground. Hold the stretch for 30 seconds. Do not bounce. Do one set with knee straight and another with the knee slightly bent.
To stretch your calves stand a little away form a solid structure. Lean on your forearms, head resting on hands. Bend one leg and put that foot on the ground in front of you with the other leg straight behind you. Slowly move your hips forward keeping you lower back flat. Be sure to keep your back foot heel on the ground. Hold the stretch for 30 seconds. Do not bounce. Do one set with knee straight and another with the knee slightly bent.
Advanced Achilles Tendon and Plantar Fascia Stretch
To stretch your calves stand a little away form a solid structure. Lean on your forearms, head resting on hands. Bend one leg and put that foot on the ground in front of you with the other leg straight behind you. 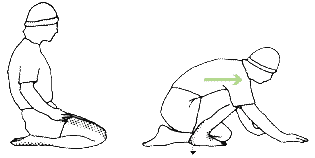 Slowly move your hips forward keeping you lower back flat. Be sure to keep your back foot heel on the ground. Hold the stretch for 30 seconds. Do not bounce. Do one set with knee straight and another with the knee slightly bent.
Slowly move your hips forward keeping you lower back flat. Be sure to keep your back foot heel on the ground. Hold the stretch for 30 seconds. Do not bounce. Do one set with knee straight and another with the knee slightly bent.
Kneel. Bring the toes of one foot almost even to the knee of the other leg Let the heel of the bent leg come off the ground a half inch or so Lower the heel toward the ground while pushing forward on your thigh. The idea is not to get the heel flat but to use forward pressure of your upper body to give and easy stretch. A very slight stretch is all that is needed. Hold for 10 seconds.
Advanced Plantar Facsia Stretch
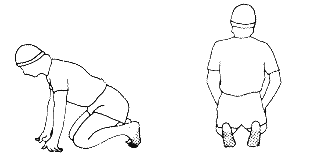 Kneel on the floor. Put your hands in front of you for balance. Slowly lean backward until you feel a mild stretch. Stretch easily for about 15 seconds.
Kneel on the floor. Put your hands in front of you for balance. Slowly lean backward until you feel a mild stretch. Stretch easily for about 15 seconds.
“Shoes should be comfortable right when you buy them,” says Jane Andersen, D.P.M., a podiatrist in Chapel Hill, N.C. “You should be able to wiggle your toes. And shoes should have a strong sole that flexes at the ball of your foot.” Consumers also should make sure that they’re wearing the right size. “Most adults don’t have their feet measured when they buy new shoes,” Andersen says, “but your shoe size can change as you get older because the feet can spread and lengthen.” Buch says one way to ensure that you get the right shoe size is to stand on a blank piece of paper and trace the outline of your feet on the paper with a pen at home. “Your shoe choice should completely cover the outline of your foot,” Buch says, “with no lines showing outside the shoe when the shoe is placed on top of the outline you traced.”
Applying moisturizing lotion on the feet after bathing can alleviate dry skin. “During dry winter months, apply a small amount of lotion a few times per day,” Kaye says. “Inexpensive generic creams are usually equally effective as expensive brand name products.” Kaye estimates that half of the ingrown toenails he treats are due to improper nail clipping. “Toenails should be trimmed straight across and not too short,” he says. “Many people incorrectly cut the corners, leaving a small point of nail that then grows into the skin or they accidentally cut the skin.”
People who pamper themselves with a salon pedicure also need to make sure that proper cutting and safety measures are followed. In the last few years, there have been ports of infections linked to nail salon whirlpool footbaths that hadn’t been properly cleaned or disinfected. Andersen suggests that people check to see that salons and their employees are licensed. “You could ask how they clean their tubs and instruments and how often,” she says. “Some people bring their own instruments.” People with diabetes should exercise caution when having salon treatments, and may be advised by their physicians to avoid treatments by anyone other than a trained podiatric or medical specialist.
To create a custom orthotic, a plaster cast is taken of your foot and sent to a laboratory. Most orthotic devices are considered “Class I exempt” by the FDA. This category means they are exempt from pre-market notification requirements. But they still must be manufactured under a quality assurance program, be suitable for intended use, be adequately packaged and properly labeled, and have establishment registration and device listing forms on file with the FDA. Legally marketed Class I devices are subject to the least regulatory control because they present minimal potential for harm to the user. But when orthotic devices make a new health claim or a claim for certain treatments, or use a fundamentally different technology, they must go through FDA clearance.
Matthew Holman, Ph.D., a scientist in the FDA’s Office of Nonprescription Products, says consumers need to pay close attention to drug labels. “Consumers should read the indications, directions, and warnings carefully,” Holman says. “A product won’t be effective if you are trying to treat a condition that’s not in the label. If it says to only use the product on intact skin with no open sores, that’s important. If a product isn’t working or the condition becomes worse, you need to seek a doctor’s advice.” People with heart disease, diabetes, and circulation problems should never self treat because of the risk of infection.
“Discolored nails aren’t always from fungus,” says Andersen. “They could also be from trauma due to exercise or psoriasis, so we take a fungal culture to make a diagnosis.” Penlac (ciclopirox), made by Dermik Laboratories of Berwyn, Pa., is an example of a topical antifungal. It is generally used daily for several months for mild to moderate nail fungus. Side effects include irritation and redness around the nails. Oral medications for fungal infections, including fungal nails and athlete’s foot, are Lamisil (terbinafine) made by Novartis Pharmaceuticals of East Hanover, N.J., and Sporanox (itraconazole), made by Janssen Pharmaceuticals of Titusville, N.J. These medicines travel through the bloodstream to attack the fungus. The tablets are taken daily for about 12 weeks. It takes about nine months for a healthy nail to grow in.
The most commonly reported side effects of the oral antifungals are headaches and stomachaches. In 2001, the FDA put out a public health advisory about both drugs and announced labeling changes. Both drugs have been associated with serious liver problems resulting in liver failure and death in rare cases. The FDA and the maker of Sporanox also warned against using Sporanox for those who have a heart condition, because of safety concerns. Patients using these drugs should immediately report symptoms of persistent nausea, anorexia, fatigue, or vomiting, upper right abdominal pain or jaundice, dark urine, or pale stools. A simple blood test is used to check liver function during treatment.
Kaye says there are two main components to bunion problems. “One problem is the pain associated with shoe pressure against the bony enlargement,” he says. “The second condition is a stiff toe joint that causes internal joint pain during movement of the big toe. Both or either of these problems can occur.” Advanced surgical techniques have improved outcomes for bunion surgery. The type of surgery needed depends on the patient’s age, activity level, and degree of deformity. Kaye says he doesn’t only remove the “bump of bone,” which won’t usually produce lasting results. “We realign the bone and use a surgical screw for stable bone alignment,” he says. Recovery time usually takes about four weeks. “The precision in which the bone is cut, shaped, and realigned is critical,” Kaye says.
Although consumers may see lasers publicized to treat bunions, lasers can’t cut bone or correct bunions, he says. Lasers are not cleared by the FDA for these indications. According to the American College of Foot and Ankle Surgeons, there have also been advances in less invasive foot and ankle surgery. Newer surgical plates and screws let surgeons repair fractures with less trauma. Smaller incisions mean less bleeding and tissue damage. In ankle arthroscopy, surgeons look at the ankle joint with a fiber optic camera system. This technique has been applied to knee surgery for several years, but now it’s being used for bones and joints in the foot and ankle. This type of surgery can relieve inflammation from arthritis and ligament damage, with reduced recovery time as compared to open surgical procedures.
Before considering any surgery, people should always explore and discuss the nonsurgical options with their doctor, and the benefits and risks of surgery. It is also important to consider the doctor’s experience and results with the procedure. The American Orthopaedic Foot & Ankle Society (AOFAS) has released statements warning about trends in cosmetic surgery to improve the appearance of the foot. “Some women are getting surgeries to shorten toes and narrow their feet so they can fit into fashionable shoes,” says Sharon Dreeben, M.D., chairwoman of the AOFAS Public Education Committee and an orthopedic surgeon in La Jolla, Calif. “A woman recently called asking if I would inject collagen into her heel, and she will probably go doctor shopping to find someone who will do it,” Dreeben says. “Some people want more padding to have cushion for high heels. But cosmetic foot surgery can result in chronic pain, infection, and nerve injury.”
Dreeben has had to fix problems from cosmetic foot surgery that went wrong. “One woman had bunion surgery even though she hadn’t been experiencing pain,” she says. “She ended up with more problems, including nerve pain and difficulty walking.” The AOFAS defines cosmetic foot surgery as surgery that is aimed at only improving appearance. Dreeben says, “Foot surgery should only be used if the goal is to provide pain relief, improve function, or enhance quality of life during normal activities of daily living. I tell people: One difference between cosmetic surgery on the face and cosmetic surgery on the feet is that you don’t walk around on your face. When you readjust one piece in the foot, it can affect everything.”
FDA approved devices for this procedure are the Ossatron, made by SanuWave Inc. of Marietta, Ga.; The Epos Ultra, made by Dornier MedTech, Kennesaw, Ga.; and the Orsabone Pain Relief System, made by Orthometrix Inc., White Plains, N.Y. People who have bleeding disorders, who are taking blood-thinning medication, or who are pregnant, should not undergo shock wave therapy. Complications can include mild neurological symptoms and tears in the tissue in the bottom of the foot.
Find out more about foot and ankle conditions on Foot Health Facts, the Official Consumer Website of American College of Foot and Ankle Surgeons.
The text presented here was originally obtained in March 2009 from the U.S. Food and Drug Administration and authored by Michelle Meadows.
Additions, modifications and deletions have been made since then for clarification and specific use on this web site.
